PERFORATED PEPTIC ULCER: GASTROINTESTINAL EMERGENCY
PERFORATED PEPTIC ULCER: GASTROINTESTINAL EMERGENCY
Having sudden onset of unbearable sharp, intense abdominal pain and a little movement is making it even more worse! And your patient have a history of acidity or ulcer! It’s an alarming situation that your patient may need an emergency consultation. It may be perforated peptic ulcer. PPU is an emergency as it lead to infection of peritoneum by leaked gastric contents. These gastric content must be sucked out by laparoscopic suction irrigation pump.
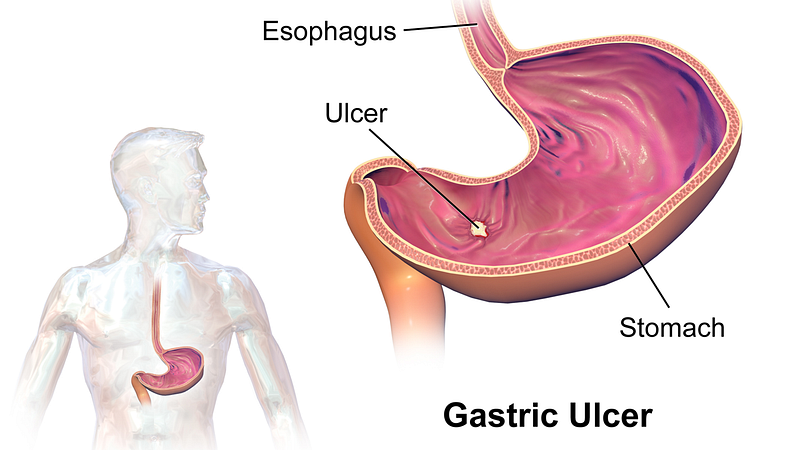
How you define perforated peptic ulcer?
Peptic ulcer is a sore or wound on the inner lining of lower most part of stomach. If it gets deep in stomach wall making a hole through it. Then it is called perforation peptic ulcer. This is a medical emergency. It can be either in stomach or duodenum.
How perforation peptic ulcer presented with?
Symptom:
a) severe pain, patient takes fetal position.
b) vomiting before starting pain.
c) feeble rapid pulse
d) cold clammy skin
e) fever
How perforated peptic ulcer happens in GI tract?
Stomach and duodenum have their own protective lining. It protects their inner lining from strong stomach acid. When the inner lining get eroded then following problem occur:
Gastritis(inflamed stomach tissue)
An ulcer(sore or wound)
Normally,peptic ulcers is caused by infection of H pylori(Helicobacter pylori). These bacteria live in the gut of people with ulcers.
Who are prone to develop PERFORATED Peptic ULCER?
“HURRY, WORRY AND CURRY”.
Bad eating habits always put in danger of developing ulcer:
- Drinking too much alcohol.
- Continuous use of NSAIDS,aspirin (which increases risk of bleeding).
- Use of carbonated drinks.
- Being on some treatments like radiation therapy, breathing machines or ulcerogenic medicines.
- Stress.
- Irregular timing of meals
- Some medical conditions.
- Trauma
How you will know it’s perforated peptic ulcer?
Prompt investigation and diagnosis can result in good outcome of treatment. Mainly, it’s diagnosis depends on following:
History from patient- complain of recurrent epigastric pain. Patient may give history of untreated corrosive ulcer or ongoing symptoms and sudden increase of pain or any recent instrumentation.
Physical examination- it shows rebound tenderness of abdomen, broad like abdomen. Fetal position of victim.
Blood investigation for serum amylase lipase, for infection etc.
Chest x-ray — it shows presence of air below the diaphragm. If history is appropriate and symptoms is exactly like PPU then chest x- Ray can justify the diagnosis. Barium meal can be done to see the pathway.
CT scan abdomen — it increases the ability of diagnosis if it is contrast CT scan.
How Perforated peptic ulcer is treated?
Overlooking the symptoms and delay in seeking medical help can be fatal.
1) MEDICAL INTERVENTION
if the diagnosis is confirmed for perforated peptic ulcer the resuscitation process to be started aggressively, stomach decompress by nasogastric suction, and broad spectrum antibiotic is started. H- pylori treatment kit can be used.
Symptomatic treatment is also started as if there is pneumoperitoneum then suction is done to relieve the tension in peritoneum, fluid maintenance etc. Ulcer has self sealing property and peritonitis may recover in 4–6 hours. If it is not solved with medication then surgical intervention is needed. As there may be leakage of gastric content or blood in peritoneum which has to be sucked out by laparoscopic irrigation pump.
2) SURGICAL INTERVENTION
Surgical option is used for PPU not responding to medical treatment and it is worsening by bleeding. The management of PPU is immediate surgery and the laparoscopy surgery has improved its treatment. Laparoscopic surgery shows good results in PPU repair.
Moreover, laparoscopic repair of PPU is done after visualizing the correct site of perforation, the leaked gastric content can be washed by irrigation pump and aspirated out by laparoscopic irrigation pump.
Small incision on abdomen made by surgeon to put laparoscopy with camera and LED light. To make more space inside co2 insufflator is used. With the help of other port and instrument surgeon repairs hole with patch.
Laparoscopy is more feaseble and easily improvable as compared to conservative open surgery.
We are here to deal with your problem by our highly equipped laparoscopy. It is equipped with irrigation pump, laparoscopic suction irrigation pump, co2 insufflator, LED light etc.
To get more info please contact us on http://www.diasurge.com/
Asherman syndrome: all you need to know.
Are you having absent periods? Getting cramps but not menstruating? And you have a history of frequent abortion, injury or any scaring. Then you may need to see a gynecologist. You may be suffering from ASHERMAN syndrome.
What is known as asherman syndrome?
Asherman syndrome is an uncommon uterine condition. In which scaring of the inner wall of uterus causing adhesion of anterior and posterior wall of the uterus. It may vary from mild to severe. Depending on areas of adhesion and type of adhesion (thick or thin). This condition leaves very little space in the uterus.
Presented with what kind of symptoms?
- absent periods or very light periods (amenorrhea or hypo menorrhea)
- severe cramps during the period date but menstruating sparsely
- unable to get pregnant
What is the cause or risk factor of asherman syndrome?
Near about 90 percent of Asherman syndrome cases occur due to dilation and curettage (D and C) procedures. D &C is usually done for missed abortion, elective abortion, retained placenta after delivery or incomplete abortion.
If a woman undergone D&C many times then it's a high risk that a woman may develop asherma syndrome.
Sometimes adhesions can happen following pelvic surgeries, like a caesarean section or surgeries of uterine or ovarian cyst, fibroid or polyp..........READ MORE
Frequent rhinitis: matter of concern.
Are you chronically suffering from blocked nose, headache, and heaviness of head? Shaking your head may worsen it. It may be due to the polyps of the nasal wall. But these symptoms occur in many other diseases. An only proper diagnosis makes it clear. Its diagnosis and treatment can be made by endoscopy.
What these nasal polyps are?
Nasal polyps are a small, painless, soft and non-cancerous outgrowth of nasal wall mucosa that occurs in the sinuses and nose. Chronic sinusitis can exist in the nasal polyp. It is not clear why it is found in some people while others don't develop polyps.
How does general health get affected by nasal polyp?
Small nasal polyps may not show any symptoms, especially a smaller one. But, larger ones can clog the sinus drainage and results in frequently infected sinuses. Chronic headache with cold and cough like symptoms. It may cause fever after sinus infection.
If they involve olfactory cells, it may cause reduces the sense of smell. Which affects daily life.
What are the symptoms present in nasal poly?
- Nose block
- Heaviness of head.
- Running nose.
- Frequent rhinitis.
- Headache.
- Shortness of breath.
- Epistaxis.

How nasal polyp get diagnosed?
Polyp's symptoms can overlap with much other illness many may be diagnosis get overshadowed.
1) Symptomatic diagnosis- on the basis of symptoms doctors can diagnose that it may be due to nasal polyp.
2) radioimaging- PNS x-ray
3) rhinoscopy (nasal endoscopy)- an endoscopy is the confirmatory examination. With the help of endoscopes, the doctor can visualize and locate the place of origin of the polyp. Thus, useful in treating it well.

How one can get rid of it?
1) You can opt for oral medicine also to make the size of polyp small or vanish. Anti-inflammatory, analgesics, antiallergic.
2) Polypectomy- surgical removal of a polyp. It is done by endoscopy.
Polypectomy Surgery:-
The general technique to remove nasal polyps is named as Functional Endoscopic Sinus Surgery (FESS). The surgeon put a narrow tube with a small camera into the nostrils and reach the sinus cavities. After that with an instrument inserted in an endoscope, a polyp is detached from the wall. With the polyp, the surgeon may clear adjacent areas in to maintain proper air entry and drainage of the sinuses. Endoscopy surgery is generally done on an outpatient basis.
Care after endoscopic polypectomy:-
After surgery doctor prescribed some antiinflammatory drugs (steroidal drugs). It is to take care that surgical removal of the nasal polyps doesn't decrease the inflammation completely so to continue the drugs given to you. Thus, improving your sense of smell by reducing inflammation of olfactory sinuses.
Don't suffer more, get your nasal issues diagnosed with rhinoscopy( nasal endoscopy), which is easy and hassle-free diagnostic procedure to cure your worry. For more information and advice consult at our website http://diasurge.com